Surgery for disc herniation is typically considered as a last resort when conservative treatments have failed to provide adequate relief. Before resorting to surgery, healthcare providers usually recommend non-surgical treatments such as physical therapy, pain medication, and epidural steroid injections to alleviate symptoms. Only when these conservative approaches prove ineffective or when a patient experiences severe or worsening neurological symptoms, surgery may be considered as a treatment option.
Why Does a Disc Herniation Cause Back Pain?
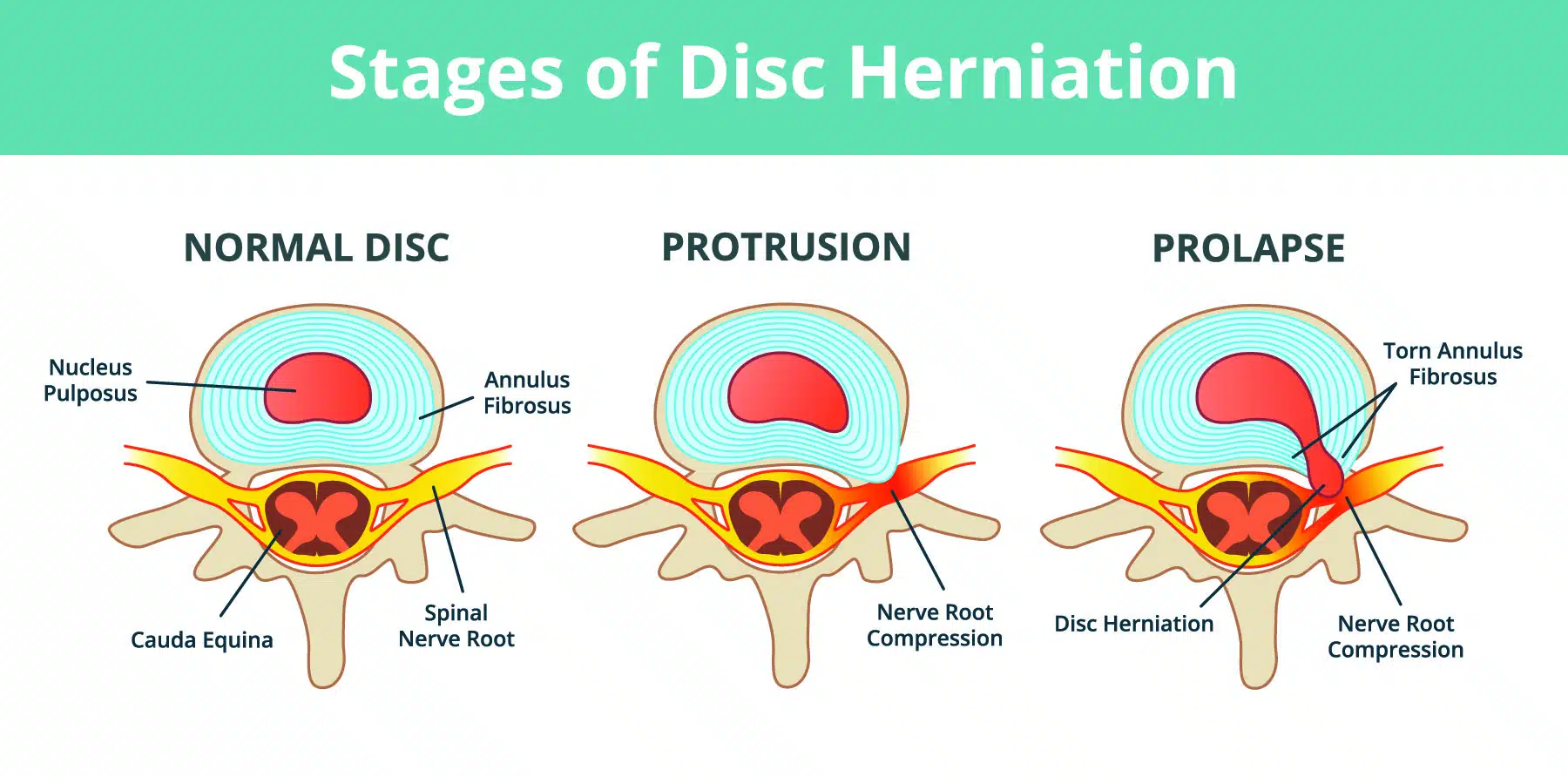
A disc herniation occurs when the soft, gel-like center of an intervertebral disc (nucleus pulposus) pushes through a tear in the tough, fibrous outer layer (annulus fibrosus). This disc protrusion can compress or irritate the nearby spinal nerves, causing pain and inflammation. The pain can be localized to the back or radiate to other parts of the body, such as the buttocks, legs, or feet, depending on the location of the herniated disc and the affected nerves.
What Area of the Spine Most Commonly Exhibits a Disc Herniation?
Disc herniations most commonly occur in the lumbar spine (lower back), particularly at the L4-L5 and L5-S1 levels. This is because the lumbar spine bears the most weight and undergoes the greatest amount of stress and movement compared to other parts of the spine. The cervical spine (neck) is another area where disc herniations can occur, but they are less common than in the lumbar spine.
When is Spine Surgery an Option for Pain Relief from a Disc Herniation?
Spine surgery is typically considered as a last resort when conservative treatments, such as physical therapy, pain medication, and epidural steroid injections, have failed to provide adequate relief. Surgery may also be recommended in cases where a herniated disc causes severe or worsening neurological symptoms, like significant muscle weakness, loss of bowel or bladder control, or difficulty walking.
What is the Most Common Spine Surgery for Disc Herniations?
The most common spine surgery for disc herniations is a microdiscectomy. This minimally invasive procedure involves the removal of the herniated portion of the intervertebral disc that is compressing the nearby spinal nerves. The goal of the surgery is to alleviate pain and other symptoms associated with nerve compression, such as numbness, weakness, or tingling in the legs or feet.
The procedure typically involves a small incision in the lower back, through which the surgeon uses specialized instruments and a microscope to access and remove the herniated disc material. Microdiscectomy has a high success rate and is generally well-tolerated, with most patients experiencing significant improvement in their symptoms after surgery.
Is a Microdiscectomy for Disc Herniation Safe?
Microdiscectomy is generally considered a safe and effective procedure with a high success rate. As with any surgery, there are potential risks and complications, such as infection, bleeding, nerve damage, and anesthesia-related issues. However, the minimally invasive nature of microdiscectomy reduces the risk of complications compared to more invasive spine surgeries. Most patients experience significant improvement in their symptoms after surgery, and the recovery period is typically shorter than with traditional open surgeries. It is important to discuss the potential risks and benefits of the procedure with your healthcare provider to determine if it is the right treatment option for your specific situation.
In summary, for a disc herniation, the most common type of spine surgery is a microdiscectomy, also known as a microdecompression or a lumbar microdiscectomy. This minimally invasive procedure involves the removal of the herniated portion of the intervertebral disc that is compressing the nearby spinal nerves, causing pain and discomfort. The surgery aims to alleviate pain and other symptoms associated with nerve compression, such as numbness, weakness, or tingling in the legs or feet.
If you are experiencing back pain or considering spine surgery, please contact a medical professional or spine specialist.