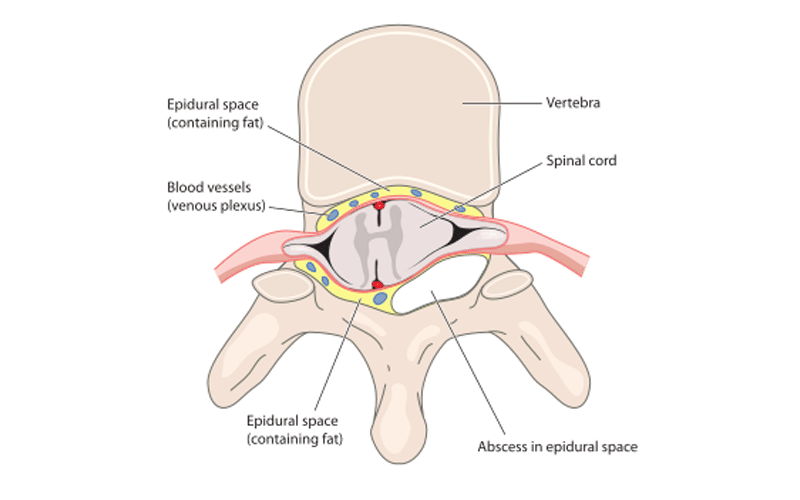
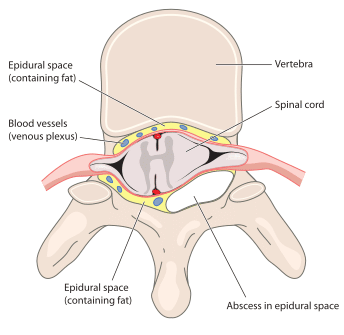
A spinal epidural abscess is a collection of pus that has formed outside the spinal cord in the epidural space. The epidural space is the area between the outer layer of the spinal cord and the bones of the spine. Symptoms of an epidural abscess may include fever, back pain, and difficulty walking. Treatment typically involves a combination of antibiotics and drainage of the abscess.
Definition
An epidural abscess is an infection that results in the collection of pus within the epidural space
The epidural space is the area between the outer layer of the spinal cord and the bony vertebrae that make up the spine. It is a thin, tube-like region that surrounds the spinal cord and runs the entire length of the spine. The epidural space contains blood vessels, fat, and a small amount of connective tissue, as well as the spinal nerve roots, which are responsible for carrying sensory and motor signals to and from the brain.
The epidural space is the site of the epidural injection, which is used to relieve pain during procedures such as childbirth.
Causes of Epidural Abscess
A spinal epidural abscess is usually caused by one of three things:
- Spread through the bloodstream (hematogenous spread): This is when the infection is spread through the bloodstream, from a source elsewhere in the body. This can occur when a skin infection or pneumonia, for example, makes its way into the bloodstream and is “seeded” into the epidural space.
- Spread through nearby structures (contiguous spread): This is when the infection is spread from a nearby structure, such as skin, an infected vertebra or intervertebral disc.
- Direct inoculation of bacteria: This is when there is direct injection of bacteria or other mico-organism into the vertebra. This can occur from trauma or as a complication from a procedure or surgery.
There are several risk factors that can increase a person’s risk of developing osteomyelitis, including:
- Weakened immune system: People with compromised immune systems, such as those with HIV/AIDS or cancer, are at increased risk of infection.
- Chronic medical conditions: Certain medical conditions, such as diabetes and end stage renal disease, can increase the risk of infection.
- IV drug use: IV drug use can introduce bacteria from the skin into the bloodstream
- Previous surgery: People who have had surgery, particularly spine surgery, may be at increased risk of developing an epidural abscess.
- Injections or spinal procedures: Procedures that involve injecting substances into the spine or manipulating the spine can increase the risk of infection.
- Use of certain medications: Some medications, such as corticosteroids and immunosuppressants, can weaken the immune system and increase the risk of infection.
Symptoms of Spinal Epidural Abscess
The symptoms of a spinal epidural abscess can vary depending on the size and location of the abscess, as well as the individual’s overall health. Some common symptoms of a spinal epidural abscess include:
- Back pain: This is often the first symptom of a spinal epidural abscess and may be severe. The pain may be constant or intermittent and may be worse when lying down.
- Fever: Many people with a spinal epidural abscess develop a fever as a result of the infection.
- Weakness or numbness: A spinal epidural abscess can compress nerve roots or the spinal cord which can cause weakness or numbness
- Loss of bowel or bladder control: In severe cases affecting the low back, a spinal epidural abscess that compresses nerve roots or the spinal cord can cause loss of bowel or bladder control.
Diagnosis of Epidural Abscess
Spinal epidural abscess is usually diagnosed through a combination of medical history, physical examination, labs, and imaging tests.
History and Physical Examination
During the examination, the healthcare provider will ask about the symptoms and the location and severity of the pain. They will ask about your medical history and any risk factors for developing an epidural abscess.
Physical exam findings may include
- Tenderness in the affected area
- Decreased range of motion: An epidural abscess may cause decreased range of motion in the affected area of the spine.
- Numbness or tingling: The infection may cause numbness or tingling in the back, legs, or arms if nearby nerves are affected.
Laboratory Tests
Lab tests may be used to help diagnose an epidural abscess and determine the cause of the infection. Some common lab tests that may be ordered include:
- Complete blood count (CBC): This test measures the number and types of cells in the blood, including red blood cells, white blood cells, and platelets. An elevated white blood cell count may indicate an infection.
- C-reactive protein (CRP) test: This test measures the level of CRP, a protein produced by the liver in response to inflammation. An elevated CRP level may indicate an infection or inflammation.
- Erythrocyte sedimentation rate (ESR): This test measures the rate at which red blood cells settle to the bottom of a tube. An elevated ESR may indicate inflammation or infection.
- Blood culture: This test involves taking a sample of blood and culturing it in a laboratory to identify the specific type of bacteria causing the infection.
Imaging Studies
Imaging studies typically used to confirm the diagnosis of osteomyelitis and to determine the location and extent of the infection. Some common imaging studies that may be used to diagnose discitis include:
- Computed tomography (CT) scan: CT scans use X-rays and a computer to produce detailed images of the spine. CT scans may show signs of infection, such as abscesses or areas of inflammation.
- Magnetic resonance imaging (MRI): MRI is the modality of choice to diagnose an epidural abscess. MRI uses a strong magnetic field and radio waves to produce detailed images of the spine. MRI is particularly useful for identifying soft tissue abnormalities, such as an abscess or nerve/spinal cord compression.
Treatment of Epidural Abscess
Treatment for spinal epidural abscess requires a combination of drainage of the abscess and antibiotics for several weeks.
Antibiotics
The specific type of antibiotics used and the duration of treatment depend on the type of infection.
Typically, antibiotics are administered intravenously (IV) for 4-6 weeks. If there is also infection of the vertebral bone (osteomyelitis), the duration may be up to 8 weeks.
Drainage
Drainage of the abscess is an important part of treatment. There are several potential methods to accomplish this.
- CT guided aspiration: During the procedure, you will lie on a table while a CT scan is performed to guide the placement of a needle or small tube into the abscess. The needle or tube is used to drain the infected fluid from the abscess.
- Surgery: Surgery is often the recommended treatment for spinal epidural abscess. A laminectomy is a surgical procedure that involves removing a small section of the lamina, the bony arch at the back of the vertebrae. This allows access to abscess and proper wash-out. Often a drain is left in place for several days to allow continued irrigation until the infection is resolved.
Prognosis
Overall, the prognosis for spinal epidural abscess is generally good with timely and appropriate treatment. In most cases, surgery to drain the abscess and remove infected tissue is effective at eliminating the infection and relieving symptoms. However, the recovery process can be lengthy, and some patients may experience permanent nerve damage or other complications.