Summary
The word “arthritis” is a medical term that refers to inflammation of the joint. Arthritis can affect any joint in the body and is relatively common in the spine. The most common type of arthritis is osteoarthritis, a degenerative arthritis caused by wear and tear. However, arthritis can also be caused by autoimmune disorders such as rheumatoid arthritis and ankylosing spondylitis. Arthritis in the spine can cause pain, stiffness, and in some cases numbness or weakness in an extremity. Treatment often includes anti-inflammatory medications and physical therapy.
What is Spinal Arthritis?
The spine is made up of 33 bones, called vertebrae, which are stacked on top of each other. Each vertebra creates a joint with the one above and below. The joint is made up of an intervertebral disc and two sets of facet joints, which connect the vertebrae with one another. These joints allow the spine to twist and bend. These joints can become inflamed in a condition knowns as “arthritis.”

Causes of Spinal Arthritis
Spinal arthritis is caused by either degenerative changes (wear and tear) or by autoimmune disorders (such as rheumatoid arthritis and ankylosing spondylitis).
Degenerative (wear and tear)
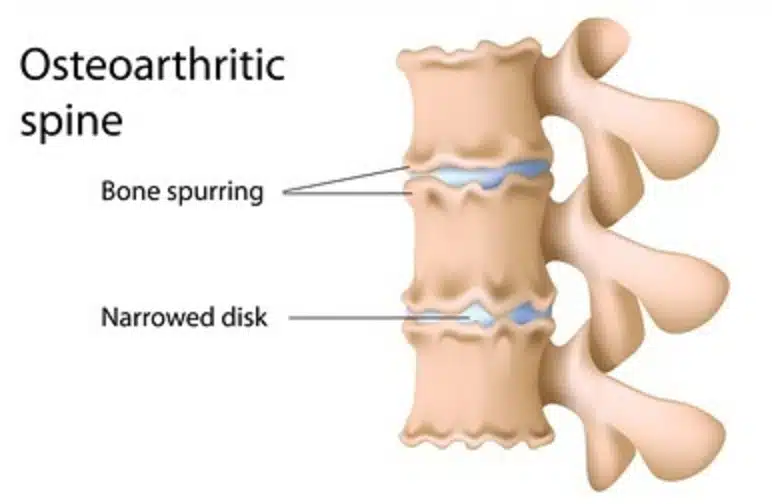
Spinal arthritis can be caused by degenerative changes which results in a condition knowns as osteoarthritis (OA). Osteoarthritis is due to general wear and tear that occurs in the spine overtime. The cartilage that makes up the facet joints can become brittle and wear down. Osteophytes, which are bony overgrowths sometimes called “bone spurs”, may form around the joint in reaction to the inflammation. Often, osteoarthritis occurs simply due to age but this condition can be accelerated by overuse or improper movements.
Autoimmune disorders
Autoimmune disorders occur when the body’s natural defense system (immune system) misidentifies its own cells as foreign and mistakenly attacks them. These disorders can result in arthritis of the spine.
Ankylosing Spondylitis
Ankylosing spondylitis is an autoimmune disorder causing chronic inflammation of the spine. In some cases, the chronic inflammation results in fusion of the vertebra. This condition is associated with the HLA-B27 antigen, a protein that can found on white blood cells in about 6% of people. However the prevalence of ankylosing spondylitis, as a condition, is 0.2% to 0.5% of people in the United States. The onset of ankylosing spondylitis typically occurs in young adulthood.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic autoimmune and inflammatory disease that can affect any joint in the body. It is the most common cause of autoimmune arthritis and typically affects the joints of the hand and feet. However, rheumatoid arthritis can also affect the spine. Although the cause of rheumatoid arthritis is unclear, it’s is believed to be a caused by a combination of genetic and environmental factors. Rheumatoid arthritis affects 0.5% to 1% of adults in the developed world.
Four Stages of Arthritis of the Spine:
- Stage 1 – is the least severe stage of OA. Patients in stage 1 will develop minor wear-and-tear in their joints, but typically feel little to no pain in the affected area.
- Stage 2 – X-rays taken at this time will start to reveal more pronounced bone spur growths (growths that often develop where bones meet each other in the joint). After prolonged periods of inactivity and seating, the affected area will start to feel stiff and painful.
- Stage 3 – The space between the bone and joint gradually narrows as the cartilage in the affected area begins to deteriorate. As a result of the inflammation, the joint begins to hurt when performing routine daily tasks.
- Stage 4 – The cartilage is almost entirely destroyed at this time, causing the joint to become inflamed. The early-stage bone spurs have now multiplied. Symptoms of pain and decreased mobility are common.
How Common is Spinal Arthritis?
Osteoarthritis (OA) of the spine is a common condition in the older population. In fact, patients over the age of sixty, 95% of men and 70% of women have at least one indicator of arthritis on imaging. However, having arthritic changes in the spine does not necessarily mean that you will have symptoms. A different study showed that osteoarthritis causes back pain in approximately 20% of men and 22% of women between the ages of 45 and 64.
Symptoms of Spinal Arthritis
Patients with symptomatic osteoarthritis of the spine typically report:
- Pain
- Stiffness
- Feeling of grinding or crunching (crepitus) when twisting or bending
Sometimes arthritis can result in bone spurs (osteophytes) which can cause nerve compression. In this case you may also experience numbness/tingling or weakness.
Symptoms depend on where the arthritis is located in the spine. Arthritis in the cervical spine (neck) will produce predominately neck and arm symptoms. Arthritis in the lumbar spine (low back) will produce back pain and leg symptoms.
Diagnosis of Spinal Arthritis
Often the diagnosis can be made clinically, meaning based on detailed interview and a careful physical examination. However, sometimes more studies are needed based on the assessment or if symptoms do not improve after initial visits.
Imaging studies
Imaging studies such as x-ray, CT scan, and MRI, are commonly used to make a definitive diagnosis or rule out other disorders that may present similarly. Each visualizes different body parts and has it’s own strengths and weaknesses.
- X-ray – An X-ray uses the passage of electromagnetic waves to create shadow like images of bones and some organs. X-rays are quick and accessible but do a poor job evaluating soft tissues such as nerves.
- CT scan – CT, also known as Computed Tomography, uses a series of x-rays along with computer processing to create detailed cross-sectional images. CT scans produce higher quality images but are still limited in their ability to assess nerves and intervertebral discs.
- MRI -which stands for Magnetic Resonance Imaging, uses a magnetic field and radio waves to create images of the body. MRI does a great job of visualizing tendons, ligaments, nerves, and intervertebral discs.
Blood tests
If a doctor suspects that the arthritis is due to an autoimmune disorder, they may order laboratory studies. These blood tests will evaluate for signs of inflammation and abnormal proteins that are markers for autoimmune disease.
Some examples of these special tests include:
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
- HLA-B27 testing
- Rheumatoid factor (RH)
- Anti-citrullinated peptide antibodies (ACPA)
Treatments for Spinal Arthritis
The treatment for arthritis of the spine depends on the underlying cause as well as other factors such as age, severity, and co-existing medical problems. Pain control and improved mobility are the main goals of treatment.
- Medication: Pain medication and anti-inflammatory medications are typically considered the first line of treatment. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be used to reduce inflammation and improve pain. If arthritis is caused by an autoimmune disorder such as rheumatoid arthritis or ankylosing spondylitis, other medications such as corticosteroids (prednisone) or other specialized medications such (such as biologics) may be indicated.
- Exercise & Physical Therapy: Directed exercises and physical therapy can help stabilize the spine, improve pain, and enhance flexibility. Some people may also find that yoga is helpful in managing their symptoms.
- Injections: Epidural steroid injections (ESI) and facet joint injections are more invasive treatments reserved for refractory symptoms. During these treatments, a specialist will use a needle to inject a mixture of pain medicine and steroids directly into the joint space. Temporary pain alleviation from injections can last weeks to months.
- Lifestyle changes: The symptoms from arthritis can be improved by maintaining a healthy weight as it will decrease the pressure from the spinal column
References:
- Kim, J. S., Ali, M. H., Wydra, F., Li, X., Hamilton, J. L., An, H. S., … & Im, H. J. (2015). Characterization of degenerative human facet joints and facet joint capsular tissues. Osteoarthritis and cartilage, 23(12), 2242-2251.
- Gellhorn, A.C., Katz, J.N. and Suri, P., 2013. Osteoarthritis of the spine: the facet joints. Nature Reviews Rheumatology, 9(4), pp.216-224.
- Laplante, B.L. and DePalma, M.J., 2012. Spine osteoarthritis. PM&R, 4, pp.S28-S36.
- Goode, A.P., Carey, T.S. and Jordan, J.M., 2013. Low back pain and lumbar spine osteoarthritis: how are they related?. Current rheumatology reports, 15(2), pp.1-8.
- Reveille JD. Epidemiology of spondyloarthritis in North America. Am J Med Sci. 2011 Apr;341(4):284-6. doi: 10.1097/MAJ.0b013e31820f8c99. PMID: 21430444; PMCID: PMC3063892.
- Goode AP, Carey TS, Jordan JM. Low back pain and lumbar spine osteoarthritis: how are they related? Curr Rheumatol Rep. 2013 Feb;15(2):305. doi: 10.1007/s11926-012-0305-z. PMID: 23307577; PMCID: PMC3606549.
- Lindsey T, Dydyk AM. Spinal Osteoarthritis. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553190/
- Sarzi-Puttini P, Atzeni F, Fumagalli M, Capsoni F, Carrabba M. Osteoarthritis of the spine. Semin Arthritis Rheum. 2005 Jun;34(6 Suppl 2):38-43. PMID: 16206956.